Identifying And Treating Pain From Nerve Tension
Nerve tension is pain that occurs because a nerve is being compressed or stuck in its surrounding tissue which prevents it from moving within its tract like it normally does. This can happen for a variety of reasons. If a joint has been immobile for a period of time it increases the risk that a nerve can get a little stuck
A great deal of emphasis is placed on maintaining flexibility in the soft tissues, such as muscle, in order to maintain optimum function and reduce injury. However, other structures or systems must also have flexibility or pliability during movement. The nervous system, which is more commonly perceived as a network of communication lines, actually needs this flexibility and pliability too.
Nerve Disorders
Injuries that occur from pressure on nerves like piriformis syndrome or carpal tunnel syndrome are the most common peripheral nerve disorders. However, excessive tensile (pulling) stress on neurological structures can also cause similar symptoms. While neurological structures can take some degree of tensile stress, too much of it will cause pathological symptoms such as pain, paresthesia (pins and needles sensations), numbness, or other disturbances of sensory or motor function. Excessive tensile stress on neurological structures is called adverse neural tension. Here’s how it plays out in the body.
The long axons of nerves in the human body include several different connective tissue layers (Figure 1). A tissue called the endoneurium surrounds each individual axon. Bundles of axons called fasicles are surrounded by another tissue called the perineurium. The entire nerve is surrounded by another connective tissue, the epineurium. These connective tissue layers of a nerve have their own nerve supply as well. If they are stretched excessively, this may produce neurological symptoms.
Cells throughout the body contain cytoplasm, an essential ground substance necessary for proper cellular function. Inside the nerve cells there is a special cytoplasm that is called axoplasm (cytoplasm of the axon). The axoplasm contains nutrient proteins necessary for proper nerve function.
The axoplasm moves throughout the entire axon and this movement of axoplasm is called the axoplasmic flow.
In addition to stretching connective tissues, excessive tensile stress applied to a nerve may cause disturbances of axoplasmic flow. These disturbances will limit the movement of essential nutrient proteins to other parts of the nerve. It is thought that the nutrient deficiency and altered axoplasmic flow are common causes of neurological symptoms such as pain, paresthesia, numbness, or motor dysfunction.
The Presence of Flexibility
Healthy functioning nerves are positioned with enough slack to lengthen and stretch to some degree, because they must accommodate movement across substantial joint angles. When there is some restriction of that flexibility, adverse neural tension results. For example, the sciatic nerve, which splits into the peroneal and tibial divisions, must be quite flexible. The nerve is somewhat slack in a neutral anatomical position with the hips in extension.
However, suppose the client is supine and moving through a straight leg raise position, as if stretching the hamstrings. In addition to stretching muscle tissue, the nerve is being elongated. If it is not fully free to slide and lengthen along its path, adverse neural tension will result and neurological sensations may be felt in the lower extremity. In some cases scar tissue from hamstring strains may tether the nerve to adjacent tissue and increase neural tension, producing the neurological symptoms.
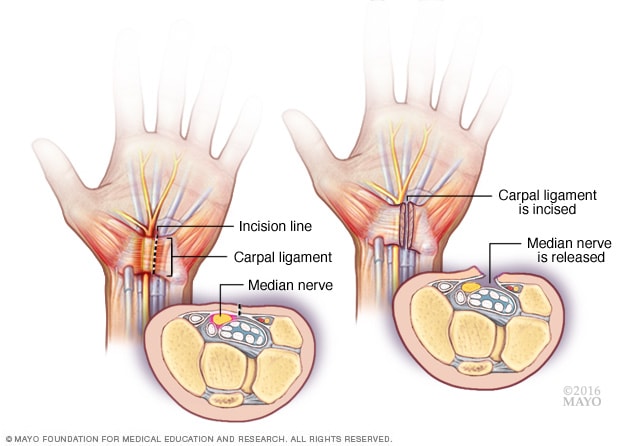
One of the primary reasons for improper neural mobility may be a problem at the region called the mechanical interface. The mechanical interface is the region involving the tissue or structure that is most anatomically adjacent to the nerve. It is this tissue that will often impact the free mobility of the nerve. For example, in the wrist, the tendons of the wrist flexors and the transverse carpal ligament would both be considered the mechanical interface. It is compression between these structures that often limits free mobility and movement of the median nerve, causing carpal tunnel syndrome.
Assessing the Problem
Identifying problems of adverse neural tension is not easy. Problems may be intraneural (within the connective tissue components of the nerve) or extraneural, such as problems with the mechanical interface. Adverse neural tension often occurs in conjunction with other problems so there is not a discrete set of signs and symptoms that will indicate excessive neural tension.
One of the common methods used to identify peripheral nerve pathology is the electromyography (EMG) test. In this procedure special electrodes are used to measure the speed of impulse transmission along various parts of the nerve. If the impulse transmission is slowed in an area there is a strong likelihood of some nerve pathology in the region. If the transmission is not slowed, the problem is thought to be elsewhere.
However, it has been demonstrated that problems with the connective tissue elements of a nerve (which have their own nerve supply) may not affect the ability of the nerve to conduct an impulse. Therefore, a person may have an EMG test that is normal, yet there are pain-producing effects from damaged connective tissues in the nerve.
There are a number of special neural tension tests that may be used to identify areas of adverse neural tension. The straight leg raise test, the slump test, passive neck flexion, prone knee bend test, and upper limb tension tests, for example, will often give additional information about levels of neural tension in peripheral nerves.
Treating Adverse Neural tension
Adverse neural tension may be treated when addressing other soft tissue problems. Many of the assessment procedures mentioned above are also used for treatment of adverse tension. The neural tension tests will put tensile stress on the nerve structures. If this is done repeatedly it may make them less sensitive to excessive amounts of tension and may in fact help stretch some of the connective tissue components of the nerve, making it less likely to produce symptoms.
It may seem contradictory to stretch the nerve for treatment since it reproduces symptoms. However, if the stretch is done gradually and frequently within the client’s comfort tolerance, it will often improve the symptoms. Treatments for interfacing structures such as muscles, joints, fascia, and skin are also likely to be helpful, as are postural and/or ergonomic changes.
While most massage therapists don’t see treatment of the neurological system as a primary function that they perform, it is evident that the nervous system is involved in many pathological processes. A greater knowledge of the anatomy and mechanics of these structures may help alleviate problems in many cases that have persisted after significant interventions that should have helped.